Background
Osteochondritis Dissecans (OCD) lesions sometimes do not heal despite initial treatment, surgical or non-surgical, to save the OCD fragment. This can result in a hole or defect on the surface of the joint where the cartilage and bone are either missing or damaged beyond repair. If the size of the lesion is large enough and is left untreated, it can lead to further joint deterioration. This may result in an increase in size of the lesion as well as damage to surrounding bone and cartilage, leading to further joint degeneration (arthritis). In order to prevent the progressive changes, the lesion area will typically need to undergo a surgical procedure to restore the joint surface.
Treatment options for bone and cartilage lesions from OCD include both nonsurgical and surgical methods. Non-surgical techniques may include restriction of activities and/or non-weight bearing on the affected limb; joint injections with stem cells or lubricating agents (viscosupplementation); or use of oral supplements including chondroitin sulfate. These non-surgical measures have limited effectiveness in larger lesions, which is typical of OCD lesions. The goal of surgical intervention is to restore the joint surface in order to eliminate pain and recover function, allowing a return to activity and sports. Ideally this improvement should last many years and hold up to the demands of all activity. Your physician will discuss with you the options for treatment and recommend a treatment plan based on your specific situation.
Surgical Options
1. Structural biologic tissue replacements
Structural biologic tissue replacements consist of harvesting bone and cartilage (osteochondral grafts) to fill the defect. The two main options are grafting tissue from the same individual (autograft) of from a different individual (allograft).
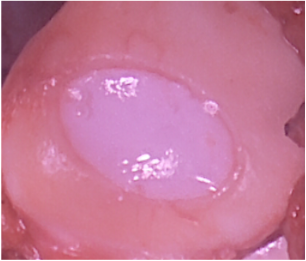
Osteochondral autograft transfer (OAT) is used to fill small to medium sized defects (Figure 1) and osteochondral allografts (OCA) are used to fill large defects (Figure 2). Autografts come from some other location in the joint of the patient being treated. Autografts provide the benefit of more predictable healing and lower cost, but are limited in the size of lesion that can be treated. Allografts are harvested from a recently deceased individual (organ donor) and must be transplanted within a few weeks from the harvest date. Allografts provide more tissue for transfer and are therefore used to treat larger lesions; allografts are associated with a higher cost. Both OAT and OCA provide normal structural architecture of the bone and cartilage in contrast with nonstructural biologic tissues, which do not have the same histologic appearance of the cartilage.