OCD definition
OCD, also known as osteochondrosis/osteochondritis dissecans, is a disease of the developing joints that is most often seen in young, growing patients. In addition to humans, this condition has been described in several domestic animal species, including dogs, horses, and pigs. The disorder is characterized by the formation of cracks, flaps, and/or loose bodies, composed of cartilage and underlying bone, within the affected joints. OCD lesions in humans most often develop in the knee joint and less frequently involve the elbow and ankle joints.
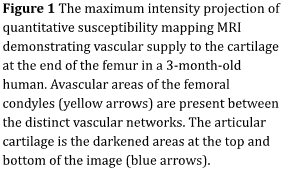
In this handout we will provide you with MRI and histology images that illustrate current thoughts about the most likely pathway for the development of OCD and its progression to clinical disease.
How does OCD develop?
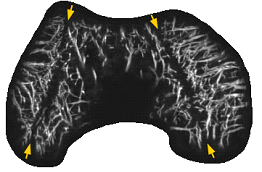
The details of the development of OCD remain incompletely understood, but recent studies performed in human and animal patients indicate that the development of OCD lesions starts well before the appearance of clinical signs, such as pain. Early in development, the ends of the growing long bones are composed entirely of cartilage. The surface articular cartilage, which provides the smooth gliding surface of the tissue, obtains its nutrition from the synovial fluid. Conversely, the remainder of the end of the growing long bone is composed of epiphyseal (also known as “growth”) cartilage which requires a blood supply to maintain its viability (Figure 1). During growth, the epiphyseal cartilage is gradually replaced by bone in a process known as endochondral ossification. In adults, the only cartilage remaining is the surface articular cartilage. It is believed that the development of OCD starts with a disturbance of the blood supply to the epiphyseal growth cartilage which results in an area of the epiphyseal growth cartilage dying. This prevents replacement of the epiphyseal growth cartilage with bone via endochondral ossification.